What is Endometriosis?
Endometriosis is a remarkable and unusual condition affecting millions of women throughout their reproductive years. Tissue normally forming the lining of the uterus, the endometrium, migrates via an unknown mechanism outside of the uterus and establishes “islands” of endometrium in other tissues and organs. The tissue continues to respond to the reproductive hormones just as though it were within the uterus. That is, during the early phase of the menstrual cycle, the endometriosis thickens and grows. During the latter phase of the menstrual cycle when bleeding occurs, the endometriosis bleeds as well.
Endometriosis has been found all over the body, but it is most commonly found in the pelvis, including the ovaries, fallopian tubes, the uterus, the bladder, the abdominal wall, and the intestines. It can cause an intense inflammatory
response leading to scarring (adhesion formation), tissue damage, and pain.
Endometriosis generally causes infertility in two ways.
- First, it may block the fallopian tubes by implanting directly within or around the tubes. When this occurs, the sperm cannot traverse the length of the tube to fertilize the egg in the fimbria, or distal most end of the tube adjacent to the ovary.
- Second, and this method is much less well understood, it is thought that the endometriosis effects the peritoneal fluid within the pelvis in such a way that the fluid becomes toxic to sperm and egg. This method is thought to involve complexities within the immune system and the body’s inflammatory response.
Symptoms
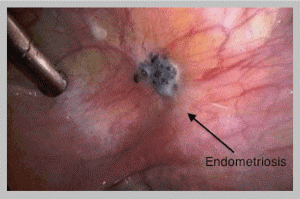
Many women with endometriosis experience painful menstrual periods, pelvic pain outside of their menstrual periods, and/or pain with intimacy. However, many women experience only the inability to become pregnant related to having endometriosis. Importantly, the absence of pain does not mean one does not have endometriosis. The only way to know for certain if one has endometriosis is to look inside the pelvis. This is accomplished via an outpatient surgical procedure called laparoscopy. Endometriosis cannot be visualized with ultrasound, CT scan, or MRI scan. In some cases, endometriosis may form large cysts filled with a liquid version of the endometriosis, called “chocolate cysts,” and this can be visualized with ultrasound and other technologies, however, this is not specific for endometriosis and requires further investigation to confirm the disease.

Surgical Treatments

Endometriosis should be considered a surgical disease, that is, it is most successfully and effectively treated with surgery. More specifically, for the best long-term results and for the greatest probability of achieving pregnancy, endometriosis should be resected or cut out. The endometriosis implants visualized at the time of laparoscopy may exhibit a “tip of the iceberg” phenomenon in that the lesion may extend deep within surrounding tissue. Burning or cauterizing the implants, while much less difficult and time-consuming, is ineffective at treating the disease. For the best results, in terms of both pain control and fertility, the disease must be completely resected and the defects created by the resection carefully repaired using microsurgical techniques to prevent adhesion (scar) formation.
Surgical management of endometriosis is most readily accomplished utilizing the da Vinci® robotic surgical system. However, there are times, albeit uncommon, when the extent of the disease and involvement of pelvic organs is such that a more conventional type of surgery known as a laparotomy is required. There are times, with very advanced endometriosis, requiring extensive surgical resection when closure of the tissue defects is impossible. In these cases it may be necessary to cover the uterus, fallopian tubes, and ovaries with a Gore-tex® “blanket” to prevent other tissues from adhering and potentially damaging the very delicate fallopian tubes. When this method is utilized, depending on the size and location of the graft material, it may be necessary to return to surgery approximately 14 days later and remove the Gore-tex®. The skill and experience of the surgeon is critical in the diagnosis and treatment of endometriosis. Finding the disease requires a very thorough investigation of the entire pelvis and abdomen as well as the ability to recognize the various and sometimes subtle changes associated with microscopic disease. It is not at all uncommon for us to find endometriosis in women who have undergone previous laparoscopic surgeries and were told they did not have the disease. Treatment of relatively minimal disease may be accomplished by most gynecologic surgeons; however, treatment of extensive disease requires considerable skill, expertise, and above all, the willingness to spend the hours necessary in surgery to adequately treat the disease.
Endometriosis, unfortunately, should also be thought of as a recurrent disease. That is, one should assume the disease will return over time. Following successful resection of all endometriosis and confirmation of open fallopian tubes, the following 6-12 cycles offer the best opportunity for conception. After that period of time, assuming all else is normal, we generally assume the disease has returned and discuss the need to repeat laparoscopy.
Non-Surgical Treatments
There is a non-surgical alternative treatment for endometriosis utilizing the drug Lupron®.
This medication prevents the normal signal from the brain to the ovary to produce a follicle and thereby estrogen. Endometriosis is dependent on estrogen and in its absence the endometriosis tends to deteriorate, completely resolving in some cases. Lupron® is given via a monthly injection and is rather expensive, although most insurance companies will cover the cost. It can be associated with an array of side effects related to the absence of estrogen including hot flashes, depression, vaginal dryness, and reduced bone density if used long-term. We don’t often utilize Lupron® in treating endometriosis for fertility related problems, but it does have a role in the management of this unusual disease.


Many physicians will recommend the use of oral contraceptives (OCPs) for the treatment of endometriosis and this is problematic for a variety of reasons. Most importantly, oral contraceptives do not cure the disease and do nothing to improve fertility (reference: www.endometriosis.org). Specifically, hormonal therapy with OCPs has not been shown to stop the disease from continuing and causing potentially irreversible damage to the fallopian tubes and other structures. OCPs can be effective in the treatment of pain related to endometriosis for the woman in whom fertility preservation is not a concern. It is very common for a young woman to be started on OCPs to address heavy, painful menses and to continue that therapy for a decade or more only to later learn she has extensive endometriosis with irreparable damage to her reproductive organs. If endometriosis is suspected a diagnostic laparoscopy is essential in confirming this life-changing diagnosis. Moreover, it is critical that endometriosis be completely resected early in the process so as to prevent permanent damage to the delicate fallopian tubes.
In Summary
Millions of women suffer from the effects of endometriosis. In the diagnosis and treatment of endometriosis it is critical to take a comprehensive, aggressive, fertility-preserving approach by providers with the skill, expertise, and temperament to take on this potentially devastating condition.
