Our Approach
This document presents our approach to the devastating problem of recurrent pregnancy loss; it is not the standard approach. Admittedly, it reflects our bias in favor of protecting life at every possible opportunity. We know life begins at the very moment sperm and egg unite and we want to be aggressive in ensuring we do everything we can to protect a growing baby.
While it is unclear how often pregnancy ends in miscarriage, it is thought to be approximately 20% of all known pregnancies. It is our impression at the Fertility and Midwifery Care Center (FMCC) that our patients do not experience this high rate of loss, presumably because of our aggressive efforts at preventing recurrent pregnancy loss (RPL) through testing and treatment of known causes.
Recurrent pregnancy loss is a controversial topic, with little agreement among medical professionals as to how it should be approached. Most providers do not recommend RPL testing until a woman has experienced two or three losses. At FMCC we consider testing after the first loss in most cases. Deciding which tests to perform and which treatments to offer following testing are also topics causing considerable disagreement among experts.
Common Causes
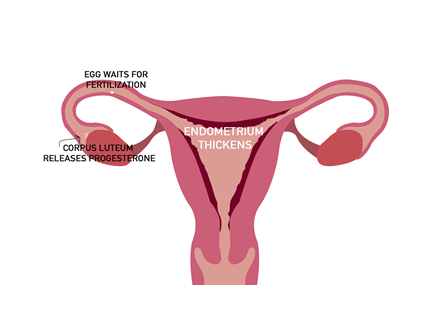
Luteal Phase Defect and Low Progesterone
Progesterone is produced by the corpus luteum within the ovary following ovulation. It stabilizes the lining of the uterus (called the endometrium), in addition to other important functions. If the ovary is not producing sufficient progesterone early loss may occur. When we know a luteal phase defect exists prior to pregnancy we use supplemental progesterone during the luteal phase of the menstrual cycle. In women who become pregnant and have a history of prior loss and/or any number of other pregnancy complications, we recommend immediate supplementation with progesterone and follow our modified progesterone protocol originally researched and created by The Pope Paul VI Institute in Omaha, Nebraska.
Blood Clotting Abnormalities
There are three main blood clotting genetic abnormalities, or mutations, thought to play a part in RPL. These mutations play a role in the metabolism of folic acid and the production of homocysteine, impacting the normal blood clotting process resulting in the blood being slightly more likely to clot. They are diagnosed using a simple blood test.
MTHFR
There are two common MTHFR mutations: A1298C and C677T. In general, C677T is thought to be the more clinically relevant. As we have two copies of each chromosome it is possible to have one or two copies of a mutation. Generally, two copies of a mutation are more significant than one. Women with these mutations may be more likely to experience heart attack and stroke in addition to RPL. Treatment during pregnancy for women with these mutations includes a combination of baby aspirin, a special form of folic acid known as methyl folate, and sometimes the blood thinner heparin (or lovenox).
MTHFR Supplement Treatments
Metafolate Vitamin
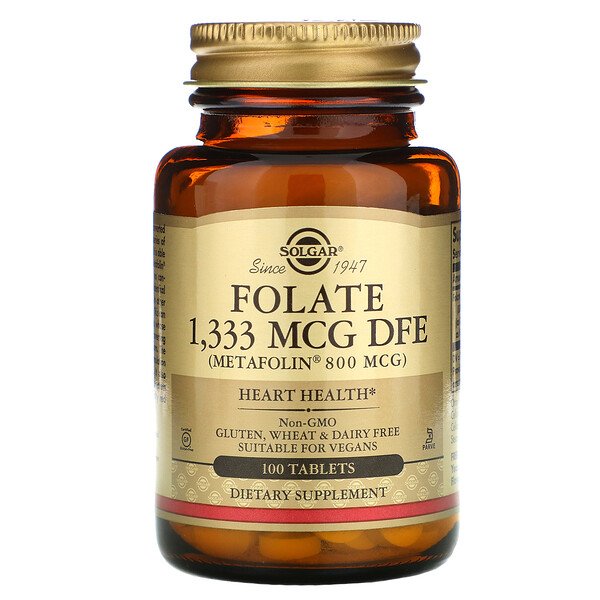
Solgar Folate Metafolin Folic Acid 800mcg, 100ct. Take two (2) by mouth everyday.
Metafolate Vitamin

Thorne Research 5-MTHF 1mg, 60ct. Take one (1) by mouth everyday.
Supplemental Metafolate Vitamins (broken down Folic Acid) can be purchased at any Healthkick store or online at www.iherb.com.
Factor V Leiden Deficiency
Factor V is one of several components of the blood clotting system and this mutation increases the likelihood of forming blood clots as well as increased risks of heart attack and stroke. Treatment during pregnancy for women with this mutation consists of baby aspirin and heparin (or lovenox) therapy.
Pai 4G/5G
This is a protein that inhibits the function of platelets, critical components in the blood clotting cascade. A mutation in the process that inhibits platelet’s function can lead to over activity of the clotting mechanism and subsequent clot formation. In general terms, the Pai mutation is thought to amplify the MTHFR mutations. That is, alone, the Pai mutation may not be clinically significant, however, when coupled with the MTHFR mutations it may serve to make the given MTHFR mutation more clinically significant. For example, we may suggest no treatment for someone with a single copy of MTHFR A1298C. However, we would likely suggest treatment if that mutation were combined with the Pai 4G/5G mutation.
Autoimmune Disorders
Most commonly referred to as Antiphospholipid Antibody Syndrome (APS), this category involves problems when the immune system over-reacts to certain proteins in the blood and other tissues, including a growing baby. This can lead to blood clots, pre-eclampsia, and recurrent miscarriages. APS is diagnosed via blood testing and is treated with baby aspirin, usually heparin (or lovenox), and sometimes steroids.
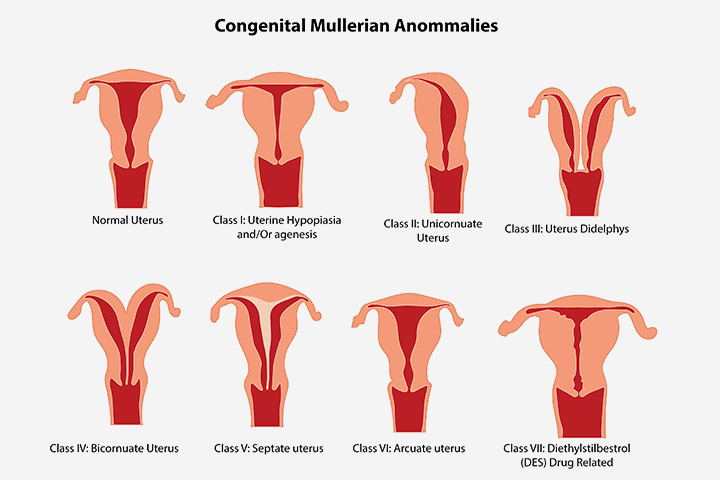
Uterine Structural Abnormalities
There are a variety of structural anomalies within the uterus that can cause problems with implantation of the embryo and proper nutrition/support of the growing fetus. A uterine septum (a wall or membrane dividing the uterine cavity) is an example of one such structural anomaly. Uterine fibroids, benign smooth muscle tumors of the uterus, are also examples of structural anomalies that can lead to pregnancy loss and other problems. Generally, these anomalies are diagnosed by ultrasound and sometimes hysteroscopy (the insertion of a small camera into the uterine cavity), and repaired surgically.
Genetic Abnormalities
This is the probably the most difficult cause of RPL in that there is no “treatment” for this type of loss. With losses in this category, from the very first duplication and division of the chromosomes when sperm and egg meet there are mistakes in the process leading to pregnancy loss. This is often referred to as a “biological loss,” or the “biological loss rate.” The probability of a loss of this type gradually increases as a woman ages. A loss in this category is more common in a 45 year old than in a 35 year old, than in a 25 year old, for example. Losses from this cause will always be with us; they are simply part our human biology.
Treatment
Treating RPL is controversial among OB/GYN providers. The American College of Obstetricians and Gynecologists (ACOG), for example, recommends against testing for the MTHFR mutations. ACOG’s position is not supported by many infertility/RPL experts, however, and even among those who agree that testing for these mutations is appropriate, there is a lack of research-based data to direct treatment. For example, to our knowledge there is no good research available to suggest that heparin (or lovenox) plus baby aspirin is superior to baby aspirin alone. We try to assist our patients in making treatment decisions taking into account their specific medical and pregnancy circumstances.

Regarding heparin (or lovenox) some would question its use in pregnancy and therefore it deserves some explanation. When treating the conditions described we use what is known as a “prophylactic” or “preventative” dosage of the blood thinner. This dosage does not increase the likelihood of bleeding. This is not true when using heparin to treat an existing blood clot such as a deep vein thrombosis (DVT) or a pulmonary embolus (PE) as much higher dosages are necessary. Heparin is given via an injection twice daily, very similar to an insulin injection for diabetes. When using heparin it is necessary to test the blood periodically, evaluating the blood clotting factors and the platelets. There is another form of heparin known as “low molecular weight heparin” or “lovenox” that may be used as an alternative. It is given only once daily and it is not necessary to perform blood testing when using this form of heparin. It is considerably more expensive than traditional heparin, yet it is usually covered by insurance plans. There are some precautions related to the timing of birth if an epidural or spinal block is required in patients taking heparin or lovenox. This is something we discuss early on in the pregnancy and plan accordingly.
Chronic Endometritis
As its name suggests, this is a chronic inflammatory condition of the uterine lining, the “endometrium”. Commonly confused with endometriosis, chronic endometritis is its own unique condition but often is found in women who also have an endometriosis diagnosis.
No less problematic, chronic endometritis often contributes to a range of signs and symptoms that are challenging for women including unusual bleeding patterns, heavy menstrual flows, intense pelvic cramping pain, painful intercourse, recurrent vaginal infections, infertility, recurrent miscarriage and other pregnancy complications such as preterm rupture of membranes and preterm labor/birth (often extreme prematurity).

The condition is not well known by most gynecologists, but is more often searched for by fertility specialists because it is so commonly seen in women struggling with fertility challenges including infertility and/or recurrent pregnancy loss. In fact, it is estimated that up to 50-60% of women with recurrent miscarriage and/or problems achieving pregnancy have chronic endometritis contributing to their fertility challenges. It is not limited to causing only fertility challenges, so sometimes searching for this condition for the cause of non-fertility problems is necessary. Diagnosing and effectively treating this condition improves symptoms, cycle health and pregnancy outcomes for women.
A combination of hysteroscopy (uterine scope), endometrial biopsy (tissue sample of the uterine lining) with request for special pathology staining, and endometrial cultures are utilized to make the diagnosis and to follow whether or not treatment is effective.
Most cases are “infectious” in nature, meaning the inflammation present is caused by a low grade infection. Most infections appear to be bacterial in nature, but sometimes fungal infections can cause this condition as well. The most common types of bacteria known to cause these infections are often normally found in the intestinal tract, though how the bacteria are able to make their way into the uterus is not yet known. Treatment is typically with antibiotic or antifungal therapy. Often additional anti-inflammatory approaches and therapies aimed at balancing the uterine microbiome are also utilized, such as probiotics.
Scientists and physicians are still learning & doing research to better diagnose and understand the condition to help determine the most effective therapies, especially for persistent/refractory cases.
